The mission of the Florida Lyme Disease Association is to improve the prevention, diagnosis, and successful treatment of lyme and related vector borne disease through education of the public and healthcare providers and support of scientific research.
![]()
LYME BASICS
 The CDC now estimates there are 476,000 new cases of Lyme disease in the United States each year. Lyme disease is caused by a spirochete (spiral shaped) bacteria (Borrelia burgdorferi) and is transmitted by certain species of black-legged ticks, and potentially the lone star tick commonly found in southern states like Florida.
The CDC now estimates there are 476,000 new cases of Lyme disease in the United States each year. Lyme disease is caused by a spirochete (spiral shaped) bacteria (Borrelia burgdorferi) and is transmitted by certain species of black-legged ticks, and potentially the lone star tick commonly found in southern states like Florida.
The nymphal, or immature, form of the tick, which is about the size of a poppy seed, causes most human cases. Because the bite is painless, many people do not realize they have been bitten. Furthermore, ticks harbor many other diseases that can be transmitted to humans aside from Lyme disease, including other bacterial infections, viruses or parasites. Indeed, there are many diseases (some life-threatening) carried by ticks that can complicate tick-borne disease diagnosis, treatment and recovery, including Babesiosis, Tularemia, Anaplasmosis, Mycoplasma, Ehrlichiosis, Rocky Mountain Spotted Fever, Borrelia miyamotoi, Bartonella, Bourbon Virus, Heartland Virus, Powassan disease among others.
Lyme and tick-borne diseases are prevalent across the entire United States. Fewer than half of patients with Lyme disease recall a tick bite. Likewise, fewer than half of patients with Lyme disease recall any rash. Although the bulls-eye red rash is considered a classic sign and warrants a clinical diagnosis, it is not the most common dermatologic manifestation of early Lyme infection. Atypical forms of this rash are actually far more common.
Infection with Lyme disease bacteria alone can lead to early symptoms such as severe headaches, debilitating fatigue, joint pain, and skin rashes, while long-term symptoms can lead to problems related to the central nervous system, including the brain, as well as the heart, joints and other musculoskeletal problems. Symptoms of Lyme disease vary for each individual patient, and also vary in intensity over the course of the disease.
![]()
LYME IN FLORIDA & THE SOUTH

- Kerry Clark, PhD has documented Lyme Borrelia in two human biting ticks in Florida (blacklegged ticks and lone star ticks). See: Borrelia species in host-seeking ticks and small mammals in northern Florida. Multiple species of Lyme Borrelia have been detected in human patients in Florida using sensitive molecular methods. Infection with species/strains other than those the traditional tests are designed to detect may contribute to negative test results. See e.g.
- Lyme borreliosis in human patients in Florida and Georgia, USA
- Geographical and genospecies distribution of Borrelia burgdorferi sensu lato DNA detected in humans in the USA
- Isolation of live Borrelia burgdorferi sensu lato spirochaetes from patients with undefined disorders and symptoms not typical for Lyme borreliosis
- A divergent spirochete strain isolated from a resident of the southeastern United States was identified by multilocus sequence typing as Borrelia bissettii.
Lyme and Bartonella infection can persist for years, despite antibiotic treatment (see studies linked above) and following:
New genetic group/species of Bartonella may be responsible for a portion of Lyme-like illness in Florida and other southern states. Standard lab tests for Bartonella will not likely identify these strains.
- The CDC shows a 29.44% increase in reported cases in Florida comparing 2017-2019 data to 2022.
- A 2021 CDC Study analyzing insurance data, revealed that in states the CDC considers to be “low incidence,” only 1 in 50 cases is counted, while in high incidence states 1 in 7 is counted. See also How much does the CDC undercount Lyme cases? It depends on where you live.
- Standard lab tests for Lyme disease were developed to detect a single Borrelia strain present in the Northeast. Such lab tests fail to detect approximately half of actual cases pursuant to numerous peer reviewed studies. See Current Guidelines, Common Clinical Pitfalls, and Future Directions for Laboratory Diagnosis of Lyme Disease, United States; see also, Project Lyme. For unknown reasons, it appears as though the Florida Department of Health is not counting most CDC-positive Lyme cases. For example, in a July 2018 report (page 7), Quest Diagnostics showed an increase in Florida Lyme cases from 283 in 2015 to 501 in 2017, representing a 77% increase. In contrast, the CDC only reported 166 Florida Lyme cases in 2015 and 210 in 2017. Why are the CDC’s numbers for Florida so much lower than Quest, a single lab? In recent email correspondence, IGeneX has indicated a 48% positivity rate in Florida for 2023, which they consider high. There were 526 CDC-positive cases through IGeneX in 2023. Note that the IGeneX immunoblot has been validated by New York and other states and is covered by Medicare Part B. We do not have data for labs such as Mayo Clinic, Consolidated, ARUP, Medical Diagnostics Laboratory, Stony Brook University Medical Center, Cleveland Clinic, university and other labs which also test for Lyme disease in Florida, but we trust that the Florida Department of Health has this data available. We would appreciate transparency on these numbers.
- Canine maps show a significant increase in incidence of Lyme disease, Ehrlichia, and Anaplasma in the state. Notably, dogs are less likely to travel out of state meaning the infections are more often locally acquired.
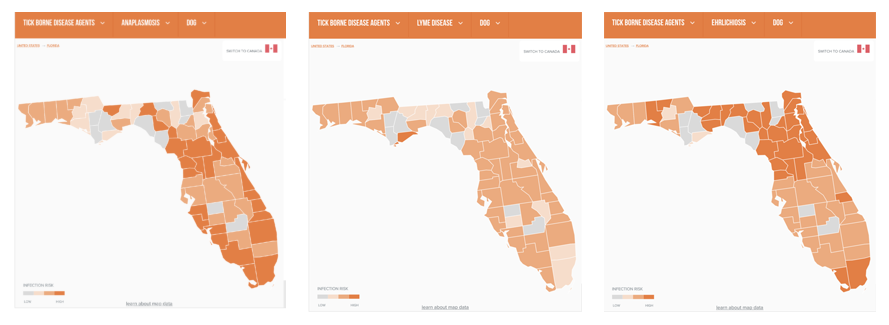
- According to the Companion Animal Parasite Council (CAPC), from 2019 – 2023, canine tick-borne infections have increased by 89.53% for Lyme disease; 100.49% for Ehrlichiosis; and 334.23% for Anaplasmosis in Florida.
- In 2022, CAPC reported 4,284 canine cases compared to only 233 human cases reported by the CDC.
- In 2023, CAPC reported 4,888 Lyme disease, 12,601 Ehrlichiosis, and 8,424 Anaplasmosis canine cases.
- According to 2024 data YTD, Florida is considered moderate risk for Lyme and high risk for both Ehrlichia and Anaplasma. Notably, the Lyme incidence changed from 1/200 in 2023 to 1/100 for 2024 YTD.
- The CAPC estimates its data represents “less than 30% of the activity in the geographic regions.” Applying this factor to the 4,284 cases in 2022, CAPC would estimate 14,280 canine cases which is >61x the human reported cases for the same year (4,284/.3 = 14,280).
- MyLymeData statistics for “low incidence” states like Florida likewise show a large disparity between reported and actual cases. See Why Doesn’t the CDC Count Lyme Disease Cases in the South and the West? Everybody Else Does. | LymeDisease.org
The one-size-fits-all IDSA treatment guidelines fail countless patients, particularly those who are not timely diagnosed/treated or present with co-infections such as Babesia, Bartonella, or rickettsial infections.
- A significant percentage of patients suffer persistent symptoms after antibiotic treatment. The CDC previously estimated 10-20% of patients, but now they claim “following antibiotic treatment, about 5-10% of people with Lyme disease have prolonged symptoms of fatigue, body aches, or difficulty thinking as a result of their infection.” We are unaware of any rationale or scientific basis for this change. To the contrary, research demonstrates a higher percentage. See e.g. Post-treatment Lyme disease syndrome symptomatology and the impact on life functioning: is there something here? (at six months, 36% of patients reported new-onset fatigue, 20% widespread pain, and 45% neurocognitive difficulties). It is widely accepted that patients who are not timely diagnosed and treated are more likely to suffer from persistent symptoms after IDSA-recommended treatment.
- Lyme persists due to biofilms, round bodies, inability of antibiotics to penetrate tissues/organs. See Lyme Persists
- Studies at Johns Hopkins showed doxycycline failed to eradicate the Lyme bacteria Borrelia burgdorferi in vitro. However, triple antibiotic combinations were effective in a mouse model. See also Superior efficacy of combination antibiotic therapy versus monotherapy in a mouse model of Lyme disease
- Studies showing “long term antibiotics are not effective” used a single antibiotic, did not have a true placebo (i.e. giving IV rocephin to the control group), and/or ignored improvement of symptoms such as fatigue. Studies were designed to fail and then were widely reported without mention of study limitations/flaws.
The failure to timely diagnose and adequately treat Lyme disease comes at a tremendous economic burden. Lyme patients had 87% more visits to the doctor and 71% more visits to the emergency room within the year following diagnosis. This does not take into account additional economic costs due to missed work and long term disability. See Johns Hopkins study Lyme Disease Costs Up to $1.3 Billion Per Year to Treat, Study Finds and Health Care Costs, Utilization and Patterns of Care following Lyme Disease | PLOS ONE; see also The Financial Implications of a Well-Hidden and Ignored Chronic Lyme Disease Pandemic – PMC
LATEST DEVELOPMENTS






